What is Glaucoma?
Glaucoma damages the eye’s optic nerve. It usually happens when the fluid pressure inside the eyes slowly rises.
Often there are no symptoms at first, but a comprehensive eye exam can detect it.
Glaucoma is a leading cause of blindness. Glaucoma can cause blindness if it is left untreated. And unfortunately approximately 10% of people with glaucoma who receive proper treatment still experience loss of vision.
There is no cure (yet) for glaucoma. Glaucoma is not curable, and vision lost cannot be regained.With medication and/or surgery, it is possible to halt further loss of vision. Since glaucoma is a chronic condition, it must be monitored for life.
Diagnosis is the first step to preserving your vision.
Everyone is at risk for glaucoma. Everyone is at risk for glaucoma from babies to senior citizens. Yes, older people are risk for glaucoma but babies can be born with glaucoma (approximately 1 out of every 10,000 babies born in the United States). Young adults can get glaucoma, too. African-Americans in particular are susceptible at a younger age.
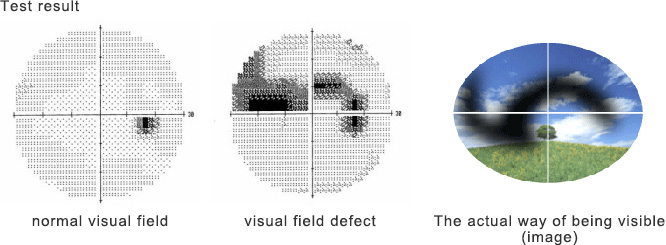
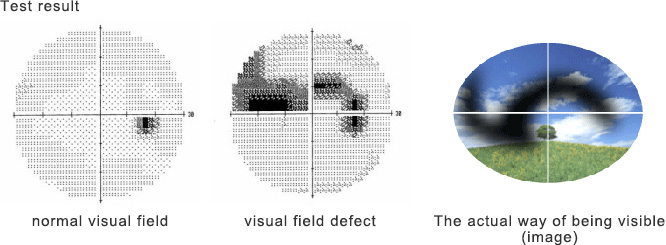
There may be no symptoms to warn you. With open angle glaucoma, the most common form, there are virtually no symptoms. Usually, no pain is associated with increased eye pressure. Vision loss begins with peripheral or side vision. You may compensate for this unconsciously by turning your head to the side, and may not notice anything until significant vision is lost. The best way to protect your sight from glaucoma is to get tested. If you have glaucoma, treatment can begin immediately.
Types of Glaucoma
Open-angle glaucoma is the most common form. Some people have other types of the disease.
1 Low-tension or normal-tension glaucoma.
Optic nerve damage and narrowed side vision occur in people with normal eye pressure. Lowering eye pressure at least 30 percent through medicines slows the disease in some people. Glaucoma may worsen in others despite low pressures.
A comprehensive medical history is important in identifying other potential risk factors, such as low blood pressure, that contribute to low-tension glaucoma. If no risk factors are identified, the treatment options for low-tension glaucoma are the same as for open-angle glaucoma.
2 Angle-closure glaucoma.
The fluid at the front of the eye cannot reach the angle and leave the eye. The angle gets blocked by part of the iris. People with this type of glaucoma have a sudden increase in eye pressure. Symptoms include severe pain and nausea, as well as redness of the eye and blurred vision. If you have these symptoms, you need to seek treatment immediately.
This is a medical emergency. If your doctor is unavailable, go to the nearest hospital or clinic. Without treatment to improve the flow of fluid, the eye can become blind in as few as one or two days. Usually, prompt laser surgery and medicines can clear the blockage and protect sight.
3 Congenital glaucoma.
Children are born with a defect in the angle of the eye that slows the normal drainage of fluid. These children usually have obvious symptoms, such as cloudy eyes, sensitivity to light, and excessive tearing. Conventional surgery typically is the suggested treatment, because medicines may have unknown effects in infants and be difficult to administer. Surgery is safe and effective. If surgery is done promptly, these children usually have an excellent chance of having good vision.
4 Secondary glaucomas.
These can develop as complications of other medical conditions. These types of glaucomas are sometimes associated with eye surgery or advanced cataracts, eye injuries, certain eye tumors, or uveitis (eye inflammation). Pigmentary glaucoma occurs when pigment from the iris flakes off and blocks the meshwork, slowing fluid drainage. A severe form, called neovascular glaucoma, is linked to diabetes. Corticosteroid drugs used to treat eye inflammations and other diseases can trigger glaucoma in some people. Treatment includes medicines, laser surgery, or conventional surgery.
Causes and Risk Factors
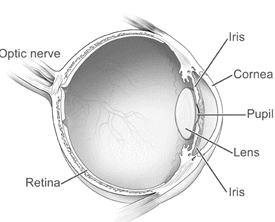
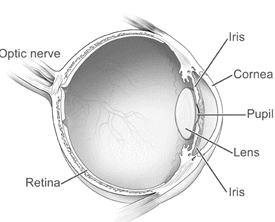
How does open-angle glaucoma damage the optic nerve?
In the front of the eye is a space called the anterior chamber. A clear fluid flows continuously in and out of the chamber and nourishes nearby tissues.
The fluid leaves the chamber at the open angle where the cornea and iris meet. (See diagram.)
When the fluid reaches the angle, it flows through a spongy meshwork, like a drain, and leaves the eye.
Sometimes, when the fluid reaches the angle, it passes too slowly through the meshwork drain. As the fluid builds up, the pressure inside the eye rises to a level that may damage the optic nerve. When the optic nerve is damaged from increased pressure, open-angle glaucoma–and vision loss–may result. That’s why controlling pressure inside the eye is important.
Does increased eye pressure mean that I have glaucoma?
Not necessarily. Increased eye pressure means you are at risk for glaucoma, but does not mean you have the disease. A person has glaucoma only if the optic nerve is damaged. If you have increased eye pressure but no damage to the optic nerve, you do not have glaucoma. However, you are at risk. Follow the advice of your eye care professional.
Can I develop glaucoma if I have increased eye pressure?
Not necessarily. Not every person with increased eye pressure will develop glaucoma. Some people can tolerate higher eye pressure better than others. Also, a certain level of eye pressure may be high for one person but normal for another.
Whether you develop glaucoma depends on the level of pressure your optic nerve can tolerate without being damaged. This level is different for each person. That’s why a comprehensive dilated eye exam is very important. It can help your eye care professional determine what level of eye pressure is normal for you.
Can I develop glaucoma without an increase in my eye pressure?
Yes. Glaucoma can develop without increased eye pressure. This form of glaucoma is called low-tension or normal-tension glaucoma. It is not as common as open-angle glaucoma.