Allergic Conjunctives

Allergic conjunctivitis can be caused by an allergy, such as an allergy to pollen (hay fever), house dust mites or cosmetics.
There are four types of allergic conjunctivitis:
seasonal allergic conjunctivitis – this affects both of your eyes and people often get it at the same time as hay fever
perennial allergic conjunctivitis – people with this type of allergic conjunctivitis have symptoms every day throughout the year in both eyes, often on waking each morning
contact dermatoconjunctivitis – this type of conjunctivitis can irritate your eyelids and it occurs most often in people who use eye drops
giant papillary conjunctivitis – this is common in people who use soft contact lenses, although it can also occur in people using hard contact lenses and after eye surgery
You might develop allergic conjunctivitis if you’re allergic to plant pollens that are released into the air at around the same time each year. This is called seasonal allergic conjunctivitis or hay fever conjunctivitis.
Perennial (all year round) allergic conjunctivitis can be caused by house dust mites or animal fur.
Eye drops, cosmetics, and other chemicals can also cause allergic conjunctivitis – eye drops are the most common cause.
You can get a form of allergic conjunctivitis called giant papillary conjunctivitis if you use contact lenses, or after eye surgery.
Self-Help
If you have allergic conjunctivitis, try to keep away from whatever is
causing the allergy.
For example if you’re allergic to a cosmetic, don’t use it again and try
an alternative product (wait until your symptoms have gone before you try
the new product).
It may be more difficult if you’re allergic to pollen, but keeping windows
and doors closed on days when the pollen count is very high may help to
reduce your symptoms.
A cool compress (a facecloth soaked in cold water) may help to soothe your
eyes.
Subconjunctival Hemorrhage
Subconjunctival hemorrhage occurs when a small blood vessel under the conjunctiva breaks and bleeds. It may occur spontaneously or from coughing, heavy lifting, or vomiting. In some cases, it may develop following eye surgery or trauma.
Subconjunctival hemorrhage tends to be more common among those with diabetes and hypertension.
Image of Subconjunctical Hemorrhage
Symptoms
1 Red, bloody patch on the white of the eye
2 Painless
3 No change in vision
Treatment
Lubricant artificial tears can soothe the eyes, although eye drops cannot
help repair the broken blood vessels.
If you are taking aspirin or blood thinners, continue taking them unless
your doctor specifically instructs you to do otherwise.
Make sure not to rub your eye, which can increase the risk of re-bleeding
right after onset ? similar to how a nose bleed is susceptible to re-bleeding
in the early stages.
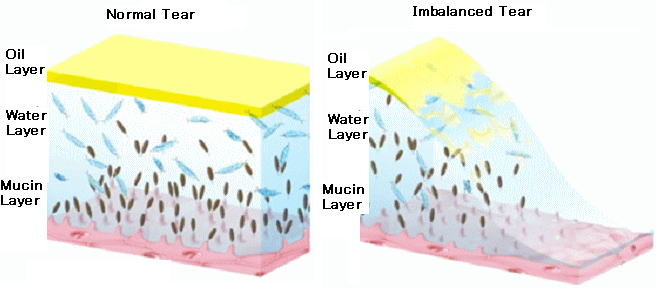
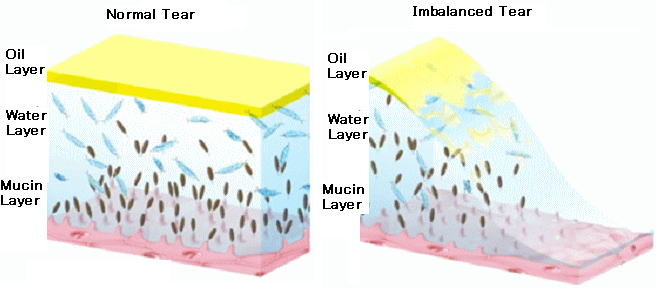
Dry Eye Syndrome
Dry eye syndrome is a chronic lack of sufficient lubrication and moisture on the surface of the eye. You can experience dry eyes when eyes don’t make enough tears or tears with the optimal chemical composition of the
three layers of the eye, which are:
The outer oily layer The middle watery layer The mucin layer
Three of the layers are all crucial to lubricating, moistening and protecting the eye. If one of these 3 layers are deficient, it is referred to as "tear dysfunction syndrome", which is essentially dry eye syndrome.
Symptoms
Persistent dryness, scratching and burning in your eyes are signs of dry eye syndrome. These symptoms alone may prompt your ophthalmologist to diagnose dry eye syndrome.
But sometimes your eye doctor may want to measure the amount of tears in your eyes. A thin strip of filter paper placed under the lower eyelid, called a Schirmer test, is one way to measure tear production.
Another symptom of dry eyes is a "foreign body sensation," the feeling that something is in the eye.
And it may seem odd, but sometimes watery eyes can result from dry eye syndrome, because the excessive dryness works to overstimulate production of the watery component of your eye’s tears.
Treatments
Though dry eyes cannot be cured, there are a number of steps that can be taken to treat them. You should discuss treatment options with an ophthalmologist.
Treatments for dry eyes may include:
1 Artificial tear drops and ointments.
The use of artificial teardrops is the primary treatment for dry eye. Artificial teardrops are available over the counter. No one drop works for everyone, so you might have to experiment to find the drop that works for you. If
you have chronic dry eye, it is important to use the drops even when your eyes feel fine, to keep them lubricated. If your eyes dry out while you sleep, you can use a thicker lubricant, such as an ointment, at night.
2 Temporary punctal occlusion.
Sometimes it is necessary to close the ducts that drain tears out of the eye. This is first done via a painless test where a plug that will dissolve over a few days is inserted into the tear drain of the lower eyelid to determine whether permanent plugs can provide an adequate supply of tears.
3 Permanent punctal occlusion.
If temporary plugging of the tear drains works well, then silicone plugs (punctal occlusion) may be used. The plugs will hold tears around the eyes as long as they are in place. They can be removed. Rarely, the plugs may
come out spontaneously or migrate down the tear drain. Many patients find that the plugs improve comfort and reduce the need for artificial tears.
4 Other medications.
Other medications, including topical steroids, may also be beneficial in some cases.
5 Surgery.
If needed, the ducts that drain tears into the nose can be permanently closed to allow more tears to remain around the eye. This is done with local anesthetic on an outpatient basis. There are no limitations in activity after having this surgery.